An Example of Mitral Valve Repair
This patient is a 55 year old female who was treated for mitral valve endocarditis (infection of the mitral valve) approximately 20 years ago. She has had a mitral valve murmur secondary to mitral regurgitation ever since. She was recommended to have mitral valve surgery over the years, but refused. Eventually, she became so limited because of shortness of breath that she finally agreed to surgery.
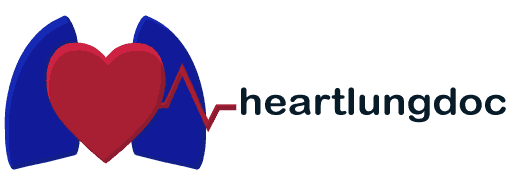
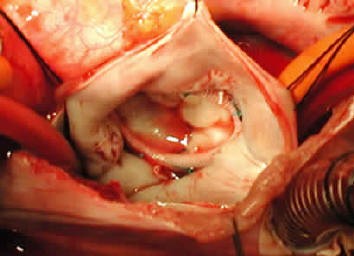
Below is a view of the outside of her heart. The large blue structure is the right atrium which in this case is massively dilated, approximately three times the normal size. The yellow structure with blood vessels going across it is the right ventricle, also severely enlarged.
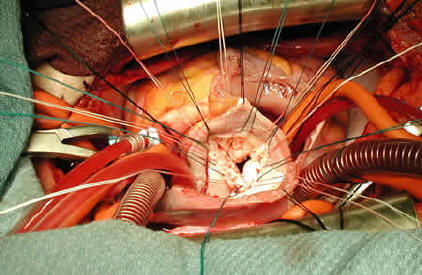
Below the right and left atria are opened exposing the mitral valve. The posterior leaflet is torn. The torn portion is being held by a surgical hook. I will excise the torn portion and repair the leaflet.
Below the leaflets are repaired. I now have placed sutures around the edges of the valve(the mitral annulus). These sutures will be placed through a ring (annuloplasty ring) that will support the repaired leaflets.
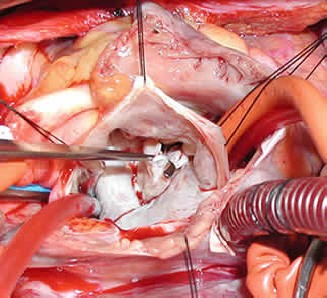
Below is the completed repair. The leaflets are sewn back together and the repair is supported by an annuloplasty ring. The patient did very well. She no longer has any leaking of her mitral valve and has returned to a normal, very active quality of life.
Below are some links to videos illustrating the techniques shown above:
In this video we’re cutting out the “flail” portion of the posterior mitral leaflet.
Here we’ve place sutures to repair the leaflet and now we’re placing more sutures to implant the annuloplasty ring.
In this final video, we’re placing the sutures into the annuloplasty ring followed by securing the ring in place around the mitral valve repair. This particular ring is known as a “flexible” ring. Annuloplasty rings come in different makes and sizes. I now more typically use a semi-rigid ring.
Why Mitral Valve Repair is Preferred Over Replacement
Mitral valve repair is generally favored over replacement, even during complex procedures like concomitant coronary artery bypass grafting (CABG) or multi-valve surgeries. Here’s why:
- Preserves Heart Function: Repair maintains the native valve and subvalvular apparatus, supporting better left ventricular function.
- Lower Risk of Complications: Compared to replacement, repair carries lower risks of endocarditis, stroke, and thromboembolism—often without the need for lifelong anticoagulation.
- Improved Long-Term Outcomes: Studies consistently show better survival and quality of life post-repair, even in high-risk or combined procedures.
- Durability with Modern Techniques: Surgical advances have made repair reliable and effective across a broad range of valve pathologies. Whenever feasible, repair is the gold standard—even in complex cardiac cases.
Testimonials – Mitral Valve Prolapse Repair
With permission from the patient to post, this 66-year-old man underwent a combined mitral valve repair operation with coronary artery bypass grafting, and radio-frequency maze procedure for atrial fibrillation.
The surgery took 5 hours. The mitral valve was successfully repaired. The patient received an arterial bypass and was able to have his normal sinus rhythm restored. He is in the ICU, awake, and doing well.
Mitral valve prolapse is one of the most common causes of mitral regurgitation, and when addressed at the right time and in the right hands, repair—not replacement—can restore normal valve function and quality of life.
A few important facts worth highlighting: Mitral valve prolapse affects ~2–3% of the population. In experienced centers, >90–95% of degenerative mitral valves can be repaired rather than replaced. Operative mortality for elective mitral valve repair is <1%. Long-term durability is excellent, with >90% freedom from reoperation at 10+ years.
What this video represents goes beyond surgical technique. It reflects teamwork, thoughtful timing, meticulous repair, and the trust families place in us during some of the most vulnerable moments of their lives.
Grateful to work alongside an extraordinary cardiac surgery team and to care for patients who inspire us every day.
39-year old patient, less than 5 hours after mitral valve repair surgery using a conventional sternotomy approach. The operation took only 3 hours from start to finish.
The patient was extubated at the end of the procedure, with little to no discomfort, requiring no medications.
The 3-minute video concludes with the intraoperative TEE findings, showing the prolapsed mitral valve, followed by the successful mitral valve repair.
With permission from the patient to post, this 63-year old man had a combination of mitral valve prolapse, atrial septal defect, and an early aneurysm of the ascending aorta that was fortunately found during his work-up for mitral valve repair surgery.
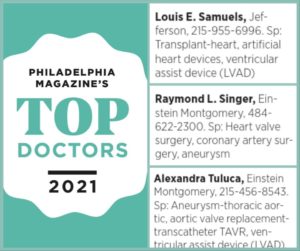
From Barto, PA, near Bally, he chose to come to Jefferson Einstein Montgomery Hospital thanks to our 99% repair rate for mitral valve prolapse and excellent outcomes.
He is ready for discharge on post-op day 4 and he describes having virtually no incisional pain.
Although not mentioned in the video, he has sung the National Anthem at the Reading Phillies and the Iron Pigs! I guess you could say we’re both “Singers!”
Mitral valve repair surgery should only be performed by surgeons who have extensive training and experience in the techniques, to allow for a successful mitral repair, instead of replacing the mitral valve with a prosthetic valve.
For a consultation or second opinion for mitral valve repair, please contact me directly at Jefferson Einstein Montgomery Hospital. I will discuss with you my 32-year experience in performing mitral valve repair, and provide you with my database of outcomes, all of which is publicly reported.
To the right you can watch a video, posted with permission from the patient, of a remarkable 63-year old cancer survivor after he underwent a right mini-thoracotomy and mitral valve repair. I and Anastasia Arce PA-C assisted Dr. Alexandra Tuluca with this surgery. It was performed at Einstein Medical Center Montgomery.
The patient was ready to go home —pain free— on post-operative day #3!
With permission to post, all smiles with Dr. Aby Augustine after his mitral valve repair and radio-frequency maze surgery for bi-leaflet mitral valve prolapse and atrial fibrillation.

TEE – Transesophageal Echocardiogram
Below you can see a case of combined mitral valve and tricuspid valve repair. This video explains the anatomy as seen on trans esophageal echocardiogram (TEE) and my techniques for repair in the operating room.
TEE using both 2D and 3D imaging has become an invaluable tool to successfully perform mitral and tricuspid valve repair surgeries. The use of intraoperative TEE is a collaborative effort by the cardiac surgeon, cardiologist, and cardiac anesthesiologist.
Below is a brief video showing a combined mitral and tricuspid repair, illustrating the importance of having a team that is experienced with intraoperative TEE 2D and 3D anatomy.
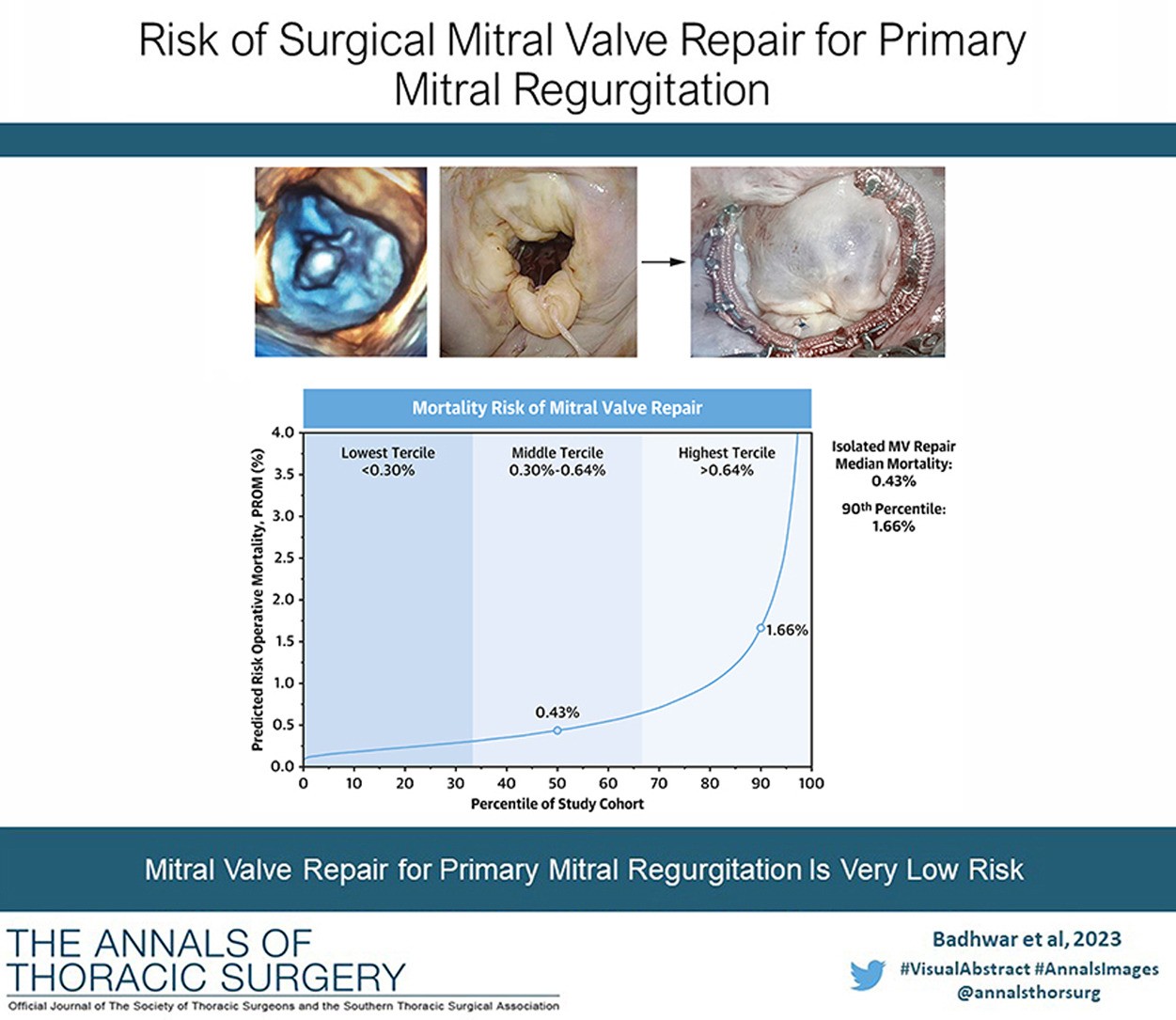
Risk of Surgical Mitral Valve Repair for Primary Mitral Regurgitation
The Society of Thoracic Surgeons (STS) has developed a new, interactive risk calculator to help cardiac surgeons and cardiologists estimate the risk of mitral valve repair for patients with mitral valve prolapse and degenerative primary mitral regurgitation (MR).
Click here to read the abstract of the article from The Annals of Thoracic Surgery.
For a consultation or second opinion for mitral valve repair, please contact us at Einstein Medical Center Montgomery – Jefferson Health.
Case Study: Complex Repair In Older Patients
Mitral valve repair surgery can be successfully performed in older patients who require concomitant coronary artery bypass surgery.
As in many patients with severe mitral valve prolapse and regurgitation, this 77-.year old patient had also developed atrial fibrillation. Therefore, we combined the mitral valve repair operation with both a coronary bypass surgery and a radio-frequency maze procedure, to correct his rhythm back to normal.
With permission from the patient to post, the patient is hemodynamically stable postop, with a well-repaired mitral valve, normal biventricular function, and his normal sinus rhythm has been restored.
In addition, as part of the maze procedure, an AtriCure clip was placed at the base of the left atrial appendage. This will allow the patient to enjoy a low risk of stroke in the future, even if the a-fib returns. In addition, the patient will no longer require blood thinners for atrial fibrillation in the future.
For patients, it’s important to know that higher volume surgeons are more likely to repair a mitral valve than to replace it, regardless of the patient’s age, or need for other procedures. This is why it’s important for patients to seek second opinions and to ask questions about their surgeon’s experience and outcomes.