Bicuspid Valve Disease
A normal aortic valve has three leaflets. In 1-2% of the population, the aortic valve is “bicuspid,” meaning it has two leaflets instead of three. This is a congenital form of heart disease, so if you are told you have a bicuspid valve, that means that you had it since birth.
Sometimes, the valve is very restricted and can even be a problem at birth. However, I typically see patient much later in life, most commonly in their 50’s and 60’s. The common story is that they have been told that they had a heart murmur most of their lives, but of late, they feel tired and short of breath.
The most common cause of symptoms with bicuspid valves is that they become calcified, causing aortic stenosis. Here again, the findings can vary. Many bicuspid valve patients have no calcium or stenosis, but instead, present with a valve that is leaking. This is particularly common in patients who present younger, in their 20’s, 30’s, and 40’s.
Another interesting aspect of bicuspid aortic valve disease is that it is often associated with aneurysms of the ascending aorta. Remember, the aorta is the large artery arising from the heart. The aortic valve and the ascending aorta are attached. It is believed that extracellular matrix (connective tissue) of the aorta is abnormal in patients with bicuspid valves. Therefore, any patient with a known bicuspid valve should have an evaluation of the aortic root by ECHO or TEE and a CT scan or MRI of their thoracic aorta.
When to Operate
The decision to operate on a patient with a bicuspid valve is the same as a patient with a normal three-leaflet valve that becomes diseased –either stenotic or insufficient. Remember, most patients with a bicuspid aortic valve can live a normal life without the need for surgery. However, if the valve becomes calcified and blocked (stenosis), or if it begins to leak a lot (insufficiency), a valve replacement may be needed.
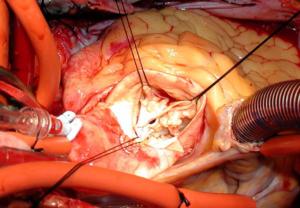
While some centers may advocate repairing a leaking bicuspid valve, or using TAVR for a stenotic bicuspid valve, I do not. The bicuspid valves that require surgery are usually very abnormal and, in my opinion, should be replaced, unless there are unique circumstances. In fact, I often say that bicuspid valve surgery is “not a rookie’s case” and should only be done by a surgeon who is experienced with bicuspid valve surgery.
I say this because I have found that patients with bicuspid aortic stenosis have a tremendous buildup of calcium that even grows into the heart muscle. It can be very challenging to remove these heavily calcified valves. For the same reason, I would not recommend TAVR for severe, bicuspid aortic stenosis.
The other issue is the aorta. Even if the size of the aorta is not aneurysmal, the aortic tissue is typically abnormal and has more of a tendency to be difficult to handle. That’s why the recommendation to replace the ascending aortic in bicuspid patients who require aortic valve replacement is as low as 4.5 cm. That is to say, if you have a bicuspid aortic valve that requires surgery, your aorta should be replaced if its size is 4.5 cm or greater. The surgeon can measure this size with a pre-operative CT scan or MRI. The ECHO and/or TEE will only show the very first part of the aorta, known as the aortic root. That is very important information, too, but to see the entire aorta, the surgeon should obtain a CT scan or MRI, prior to going to the operating room.
Not to throw a curveball at you, but if you have a normally functioning bicuspid aortic valve, you do not need your ascending aorta removed unless it is 5.0 cm or more. See below:
| A patient with a bicuspid valve needs aortic valve replacement due to stenosis or insufficiency. | If the aorta is 4.5 cm or greater, the aorta should be replaced in addition to the aortic valve.
If the aorta is less than 4.5 cm, just the aortic valve needs to be replaced. |
| A patient with a bicuspid valve does not need replacement because the valve is working fine. | If the aorta is 5.0 cm or greater, the aorta should be replaced. The valve can be left alone, so long as it is working fine and there is no calcium deposits that may suggest it will deteriorate in the next 5 years.
If the aorta is less than 5.0 cm, the patient should continue surveillance with either yearly CT scan or MRI of the aorta, along with surveillance of the valve with ECHO. |
With regards to the choice of valve, it doesn’t matter. The choices are the same –a mechanical valve versus a biologic valve. Once again, this is largely depending on age and preference. The mechanical valve will last basically for a lifetime but require Coumadin. The biologic valves do not require Coumadin but may last only 8-15 years, depending on the patient’s age –the younger the patient, the more quickly a biologic prosthetic valve will deteriorate, due to the higher metabolism of younger patients.
I’m one of the few surgeons who still advocate mechanical valves in younger patients, particularly since the CryoLife ON-X valve only requires an Coumadin INR range of 1.5-2.0 after three months. Plus, these valves are fairly quiet and most patients do not hear the clicking sound to any great degree. Conversely, I have seen a lot of patient after biologic valves (cows and pigs), return for a second operation at only 10 years, sometimes less.
The decision of mechanical versus biologic valve replacement remains the hardest decision for the patients (and the surgeons). There remains a lot of debate. Because of TAVR, most surgeons recommend a biologic aortic prosthesis, with the idea that if it deteriorates down the road, the patient can have a TAVR valve placed inside of the old prosthetic valve. This is a reasonable option, though we don’t quite yet know the durability of the TAVR valves.
Two final comments on bicuspid valve surgery. I would never perform a Ross Procedure in a bicuspid valve patient. This is due to the fact that the bicuspid valve patients have a connective tissue disease that effects the aorta, but may also effect the pulmonary arterial tissue. I don’t feel comfortable auto-transplanting the pulmonary valve and pulmonary artery into the aortic position in patients with bicuspid valve disease.
Lastly, as you know, I am not a fan of so-called “minimally invasive” aortic valve approaches, mainly because they are NOT “minimally invasive” but rather just a smaller incision, but still the same operation. This adds unnecessary risk to a very safe procedure. Please review my discussion on this matter under “Surgical Approaches.”
As mentioned above, I feel the bicuspid valve patients require more vigilance and experience in the operating room. Performing a bicuspid valve replacement and/or bicuspid aortic aneurysm operation through a small incision may increase the risk to the patient. I know that this is debated among surgeons, but my outcomes using traditional approaches remain among the best in the nation. No doubt, there are many heart surgeons who have dedicated their careers to these smaller incision techniques, some with great success. But at the end of the day, their results are not better than mine and their patients truly do not recover any sooner. Most of all, their patients are not put at less risk, but quite arguably, more risk, for undergoing the same open heart procedure –again the same open heart procedure—but through a small incision.
The good news is that patients with bicuspid valve disease do very well with surgery and can resume normal activities and enjoy a normal life expectancy.