Why is less invasive cardiac surgery a challenge?
A general surgeon performing a laparoscopic gallbladder removal in the abdomen has a lot of advantages over a heart and lung surgeon performing minimally invasive procedures in the chest.
First, the abdominal wall is soft and compliant. Second, the general surgeon will pump air into the abdomen, stretching the abdominal wall, thus forming a tent under which the surgeon has lots of room to maneuver. Lastly, the abdominal organs just sit there –for the most part, they don’t move.
Compare that to what the heart and lung surgeon faces in the chest…
The chest wall is not soft nor compliant. Instead, the heart and lungs are surrounded by a rigid rib cage and sternum. Second, we can’t pump air in the chest because it will compress the heart and great vessels causing a drop in blood pressure. Lastly, the chest organs are moving –the heart is beating, the lungs are breathing, and so on.
Rigid rib cage and sternum
A lot going on in there!
As a result, less invasive cardiac procedures have been a challenge. Because of these challenges, there have been many different approaches attempted as illustrated by the incisions shown below:
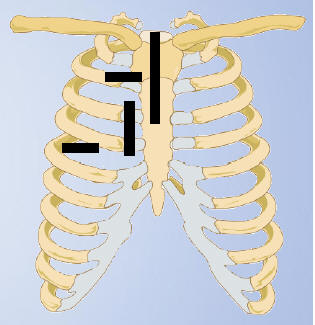
Possible Incision Sites
Let me discuss the two basic minimally invasive heart valve approaches that are being used today.
Port-Access Less Invasive Valve Surgery
Port-Access Less Invasive Valve Surgery has actually been around since the mid-1990’s. At that time it was referred to as “Heartport” after the company that first developed the technology.
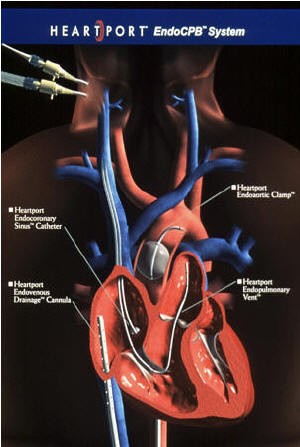
Heartport
Catheters for Heartport

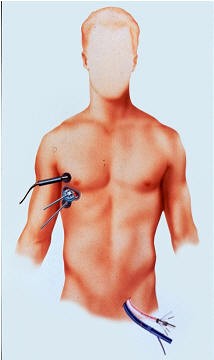
Incision in the right chest
We performed our first port-access mitral valve operation in 1997 as shown in the picture below… (I can’t believe how dark my hair was back then!)

First port-access mitral valve operation in 1997
Although we had some initial success, we soon lost some of our enthusiasm for the procedure. The technology was somewhat complex, expensive, and time-consuming. Early in our experience, we weren’t sure that the patients were doing that much better with the smaller incisions than they were with conventional techniques.
You also have to understand that less invasive procedure still can have serious complications. For example, the femoral artery in the leg can be injured. This can lead to a life-threatening condition known as “retrograde aortic dissection.”
Perhaps the most surprising thing for patients to learn is the fact that a “less invasive procedure” is actually NOT “LESS INVASIVE” In reality, it’s the same exact operation, only through smaller incisions. Many patients misbelieve that the so-called “less invasive” or “minimally invasive” procedures is somehow less of an operation. In fact, it’s often more complex.
Although the incision is smaller, the surgeon still needs to put catheters in the heart, place your body’s functions on the heart-lung machine, cool your body temperature, stop your heart, open your heart, fix your valve, close your heart, warm your body, stop the heart-lung machine, remove the catheters from the heart, and so on. In many ways, I feel they should refer to these operations as “small incision surgery” not “less invasive.”
That said, a number of surgeons throughout the country have a renewed enthusiasm for the procedure.
In part, patients continue to demand less invasive approaches. No doubt, surgeons who perform the less invasive procedures will attract more patients –and, those programs that offer less invasive approaches will grow. In other words, competitive forces have renewed the enthusiasm in the procedure as much as any real scientific advantage.
The good news is that every year there continues to be tremendous advances in instrument technology and cameras, making the less invasive procedures safer and safer.
Let’s look at some case examples:
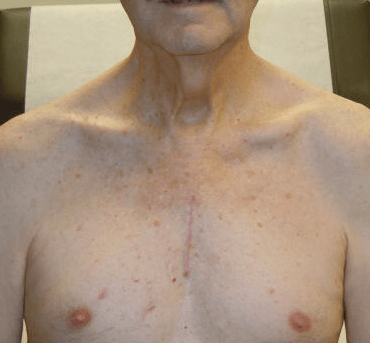
Here’s a picture of a patient who underwent mitral valve surgery through a small incision under his right breast. The picture was taken shortly after his surgery and as you can see, there’s just a small bandage below his right breast.

Small incision
Here’s another patient who underwent mitral valve repair with a small right chest incision. Note that his incision is just over his breast. The location of the incision is determined by the location of the heart on a pre-operative CT scan of the chest. The second photo is a close up of the wound only 2 weeks after surgery.

Incision is just over his breast

Close up of the wound only 2 weeks after surgery

Hidden Scar
Right Mini-Thoracotomy versus Mini-Sternotomy for Aortic Valve Surgery
There are two mini-invasive approaches for aortic valve surgery. The one is a small transverse incision between the right third and fourth ribs. This is known as a small anterior thoracotomy since the approach is via the thorax between the ribs. Below is a picture of this incision.

Small anterior thoracotomy
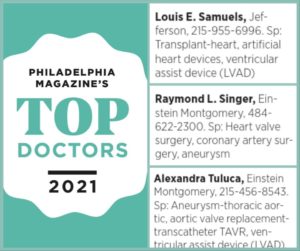
At Einstein Healthcare Network, our cardiac team is experienced in performing mini-thoracotomy procedures for patients who are born with bicuspid aortic valves that require replacement, and who are not considered good candidates for TAVR.
Through a 3-inch incision on the right side of the breast bone, we can safely replace your aortic valve without splitting your sternum or breaking your ribs, allowing for faster recovery despite undergoing open-heart surgery.
Is this small anterior thoracotomy approach less painful than a conventional sternotomy?
It’s hard to say. Patients trade sternotomy pain for rib pain, as we need to divide the 4th rib when using this approach. In a very thin patient with osteoporosis of the sternum, this approach may be better. I’ve performed a number of aortic valve replacements using this approach.
For me, it’s not ideal. The view of the aortic valve is not consistently favorable. It’s important to have a CT Scan of the chest prior to performing an aortic valve operation using this approach. The CT Scan will give the surgeon an idea of the location of the aorta and aortic valve relative to the planned incision.
However, in most patients who desire a less invasive procedure, a safer, more consistent approach is known as the mini-sternotomy. This approach is similar to the conventional sternotomy except that the surgeon only divides the upper portion of the sternum, leaving the lower part of the bone intact.
Below is a picture of a patient’s mini-sternotomy incision approximately 3 weeks after the surgery.
Mini-sternotomy incision approximately 3 weeks after the surgery
Below you can see a video, posted with permission from our patient, Robert, commenting after a successful minimally invasive aortic valve replacement, performed by my partner Dr. Alexandra Tuluca and me. This video was taken just 3 days after his surgery!
NOTE: Dr. Tuluca has focused her career on small incision surgery, TAVR, and MitraClip procedures and heads up our surgical structural heart program at Einstein Medical Center Montgomery and Einstein Medical Center Philadelphia.
So, here’s a good question: Is the mini-sternotomy incision less painful than a full, conventional sternotomy?
Guess what? It’s hard to say, again. Clearly, if you read the advertisements of surgeons who purport one technique or the other, they’ll always say how their incision “reduces pain and allows you to return to normal activity sooner.”
I truly believe it depends on the patient. That’s why I treat every patient differently. A lot of factors go into whether or not I feel you are a candidate for one technique or another. The good thing is, we have experienced in all of these approaches and therefore we can plan what’ best for you!
Below you can see a video where I discuss how minimally invasive surgery is different from open heart surgery. You can read more on TAVR here.
Discussion on Conventional Sternotomy, Mini-Thoracotomy, and Robotic Thoracotomy
There are many surgical approaches to mitral valve surgery, and therefore it can be confusing to patients who are seeking a second opinion.
The gold standard has been the sternotomy approach, providing access to all regions of the heart and the ability to do combined procedures such as multi-valve surgery, and mitral valve repair combined with atrial fibrillation surgery or coronary artery bypass surgery.
Other approaches utilize a small right thoracotomy with cannulation of the femoral artery and vein for the purpose of going on the heart-lung machine, as opposed to direct cannulation of the heart with a single incision using conventional sternotomy approach.
What many patients don’t realize is that both approaches require the use of the heart-lung machine and the stopping of the heart to repair the valve.
In robotic mitral valve surgery, a similar right thoracotomy approach is used, along with femoral artery and vein cannulation, except the surgeon looks through a camera with the robot, as opposed to looking directly through the small right thoracotomy wound. The mini-thoracotomy and the robotic thoracotomy approaches are nearly identical procedures, though the robotic involves more setup time and utilizes more complex instrumentation.
Again, all three procedures —conventional sternotomy, mini-thoracotomy, and robotic thoracotomy—are equivalent in the sense that they all require the use of the heart-lung machine to stop the heart in order to repair or replace the mitral valve.
This raises the question, what is the invasive part of a heart operation? Is it the incision? Or is it using the heart lung machine and the need to stop the heart in order to repair or replace the heart valve?
To me the answer is obvious. The invasive part of the procedure is not the incision, but the work that we do on the inside on the heart itself!
Furthermore, when performed well, the conventional sternotomy not only affords a margin of safety, but does NOT cause significant pain, as historically patients have been led to believe —especially by using unfortunate and misleading terms like “cracking the chest.” On the contrary, as seen in all my videos, my sternotomy patients have modest, not large incisions, and rarely have significant discomfort after surgery.
In short, patients in my hands, who have a well-performed standard sternotomy have excellent outcomes (< 1% mortality), short hospital stays (4.5 days) and quick recoveries, with return to driving in 3-4 weeks, with little to no pain.
Teamwork: The Key to a Successful Outcome for Complex Procedures
Because the less invasive procedures can actually be more complex, our surgeons perform these procedures together as a team. Indeed, for all of our most complex procedures (repeat operations, trans-catheter valve (TAVR) procedures, we work as a team.

Teamwork
So, what’s our approach?
There are select patients who may benefit from a less invasive (smaller incision) approach. The different reasons why one person would be a candidate and another not are too many to list here. Simply put, every patient is different. If you desire to have a less invasive approach, we will certainly evaluate you and your condition to see if you’re a good candidate. I believe that it is this “selectivity” that has allowed us to achieve good outcomes in our minimally invasive heart valve program.
Some centers feel that adding robotic technology to the port-access approach provides better visualization and allows for even smaller incisions. So, let’s look at the Da Vinci Robot System below:
The Da Vinci Robotic System (Intuitive Surgical, Inc.)
There has been an increasing amount of excitement concerning robotic surgery. The concept is that by using
The procedure is not different than port-access. In fact, it’s
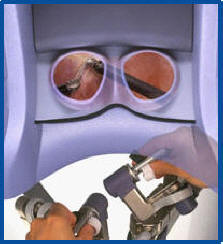
However, in addition, robotic arms and a robotic camera are placed through other small incisions to allow the surgeon to work at a distance from the surgical field. The surgeon sits at a computerized consul about 10 feet away from the operating table. Other assistants place the necessary robotic instruments into the chest as shown below:

Surgeon sitting at a computerized consul about 10 feet away from the operating table

Here’s what the robotic arms look like at the operating field
The surgeon looks into eyes of the consul

The fingers of the robot does the work
Here’s a video of what a robotic mitral valve procedure looks like up close…
The Da Vinci Robot is used extensively for lung and esophageal procedures. We have not found that the robot has added any benefit to our already successful less invasive valve procedures listed above. In addition, we feel the future of valve surgery is the new trans-catheter approach (TAVR). While it is limited to high-risk aortic valve procedures only, over the next 5-10 years the TAVR procedure will be more widely applied to most patients with aortic valve disease. Using trans-catheter techniques for the mitral valve is just around the corner as well. Stay tuned!
It’s known that robotic mitral valve surgery, as well as robotic coronary surgery, is being performed successfully at certain institutions. As discussed above, it’s not clear that these techniques are necessarily better than the minimally invasive approaches we already use.
Perhaps it’s true… the future is now.
Robot Article
To really see the future, click here to read about the Percutaneous (Trans-Catheter) approach…