Hospital Value-Based Purchasing Program (VBP)
The Patient Protection and Affordable Care Act (PPACA), often derisively referred to as “Obamare” has established a hospital value-based purchasing program whereby value-based incentive payments will be made to hospitals that meet (or exceed) performance standards.
The program has already begun (FY 2013) and will apply to payments for discharges occurring on or after October 1, 2012. Value-based purchasing (VBP) rewards high quality providers and penalizes programs for weak performance.
Beginning this year, 1% of Medicare reimbursement will be withheld from hospitals, increasing to 2% in 2017.
These funds will be redistributed to hospitals based on their performance against a growing list of “process of care measures” as well as 8 patient “experience of care dimensions.”
Hospitals that perform well in comparison to peers will receive a quality bonus, those that perform poorly will incur a penalty.
Therefore, in addition to our recognition of the importance of quality performance measures, there is now an additional incentive: getting paid!
The fact of the matter is, the government appropriately is encouraging health care providers to move from “volume to value” in the delivery of care to our patients.
“Pay-for-Performance” is here to stay and thus as health care providers it is important to understand clinical process of care measures.
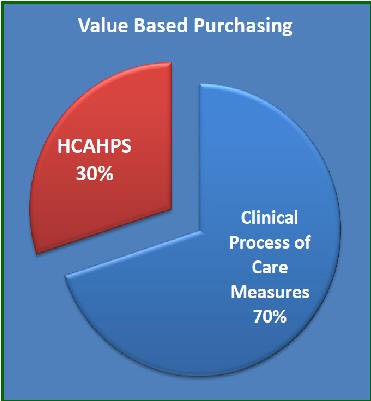
Clinical Process of Care Measures
(70% of hospital’s overall VBP rating)
Fibrinolytic therapy received within 30 minutes of hospital arrival (AMI-7a)
- Primary PCI received within 90 minutes of hospital arrival (AMI-8)
- Discharge instructions (HF-1)
- Blood cultures performed in the ED prior to initial antibiotic received in hospital (PN-3b)
- Initial antibiotic selection for CAP in immuno-competent patient (PN-6)
- Prophylactic antibiotic received within 1 hour prior to surgical incision (SCIP-Inf-1)
- Prophylactic antibiotic selection for surgical patients (SCIP-Inf-2)
- Prophylactic antibiotics discontinued within 24 hours after surgery (SCIP-Inf-3)
- Cardiac surgery patients with controlled 6 AM post-operative serum glucose (SCIP-Inf-4)
- Urinary catheter removed on POD 1 or POD 2 with day of surgery being day zero (SCIP-Inf-9)
- Surgery patients on B-blocker pre-arrival that received a beta-blocker during the peri-operative period (SCIP- Card-2)
- Surgery patients with recommended venous thrombo-embolism prophylaxis ordered (SCIP-VTE-1)
- Surgery patients who received appropriate venous thrombo-embolism prophylaxis within 24 hours (SCIP-VTE-2)
HCAHPS Survey
(30% of hospital’s overall VBP rating)
The HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey is the first national, standardized, publicly reported survey of patients’ perspectives of hospital care.
HCAHPS (which is pronounced “H-Caps”) is a 27-item survey for measuring patients’ perceptions of their hospital experience.
The Medicare Hospital Value-Based Purchasing (VBP) program links 30% of the CMS pay-for-performance reimbursement to our results on the HCAHPS survey.
Eight HCAHPS measures are employed in the hospital VBP. These include:
- Nurse communication
- Doctor communication
- Hospital staff responsiveness
- Pain management
- Medicine communication
- Hospital cleanliness and quietness
- Discharge information
- Overall rating of hospital
Hospital VBP utilizes HCAHPS scores from two time periods: —a “Baseline” and a “Performance” Period.
For FY 2013, the Baseline Period covers patients discharged from July 1, 2009, through March 31, 2010, and the Performance Period from July 1, 2011, through March 31, 2012.
The Patient Experience of Care Domain score is comprised of two parts: the HCAHPS Base Score (maximum of 80 points) and the HCAHPS Consistency Points score (maximum of 20 points).
Each of the eight HCAHPS dimensions contributes to the HCAHPS Base Score through either an “Improvement” or “Achievement” score.
“Improvement” is the amount of change in an HCAHPS dimension from the earlier Baseline Period to the later Performance Period. “Achievement” is the comparison of each dimension in the Performance Period to the national median for that dimension during the Baseline Period.
The larger of the Improvement or Achievement score for each dimension is used to calculate a hospital’s HCAHPS Base Score.
The second part of the Patient Experience of Care Domain is the Consistency Points score, which ranges from 0 to 20 points. Consistency Points are designed to target and further incentivize improvement in a hospital’s lowest performing HCAHPS dimension.
The Patient Experience of Care Domain Score is the sum of the HCAHPS Base Score (0-80 points) and HCAHPS Consistency Points score (0-20 points), thus ranges from 0 to 100 points, and comprises 30% of the hospital VBP total performance score.
All of the math aside, here is perhaps the most important thing to know… The HCAHPS results are publicly reported on the CMS Hospital Compare Website: www.hospitalcompare.hhs.gov
At the end of the day, communicating with our patients and their families in a positive and caring fashion is not only the right thing to do —it’s also paramount to our success.
Achieving Quality Control, Cost Control, and Innovation:
A Piece of Cake… Cheesecake That Is!
Dr. Atul Gawande – Professor of Surgery Brigham and Women’s Hospital – Harvard Medical School Harvard School of Public Health
Dr. Atul Gawande is a surgeon at Brigham and Women’s Hospital in Boston. He is also a Professor of Surgery at Harvard Medical School and Professor in the Department of Health Policy and Management in the Harvard School of Public Health.
He is an accomplished writer and has served as a staff writer for the New Yorker Magazine since 1998.
In the August 12, 2012 edition of The New Yorker, Dr. Gawande wrote an intriguing article reviewing the success of the Cheesecake Factory restaurant corporation and asks the question: “If restaurant chains have managed to combine quality control, cost control, and innovation, why can’t health care?”
Dr. Gawande points out that Medicine has long resisted the productivity revolutions that transformed other industries.
He concludes that our new hospital models will indeed come from industries like the Cheesecake Factory —sophisticated systems for tracking outcomes and costs, instant delivery to medical teams of up-to-date protocols, with detailed metrics on our performance.
In his comparing healthcare systems to the large restaurant chains, he asks “How soon will that sort of quality and cost control be available to patients everywhere across the country?”
Here is the link to Dr. Gawande’s interesting article:
http://www.newyorker.com/reporting/2012/08/13/120813fa_fact_gawande
And, I must admit, I love the Cheesecake Factory, too… Excellent food and service, just as Dr. Gawande describes. And, while they have some decadent items on their menu, you can find lots of healthy stuff to eat as well.
I wish they had one in Allentown. The closest ones are in King or Prussia and at the Willow Grove Mall.
Health care reform and Quality are now completely intertwined. I would be pleased to speak to your group or business on these complex and yet very important issues.