Click here to see the Trans-Catheter Valve Procedure
Healthy Mitral Valves
Let’s first consider healthy mitral valves in general.
Below is a drawing of the heart valves.
On the top of the image, the heart is cut in the so-called “coronal view” showing the vertical relationship of the four heart valves.
Beneath the coronal view, the heart is cut in the “cross-sectional view” showing the horizontal relationship of the four heart valves.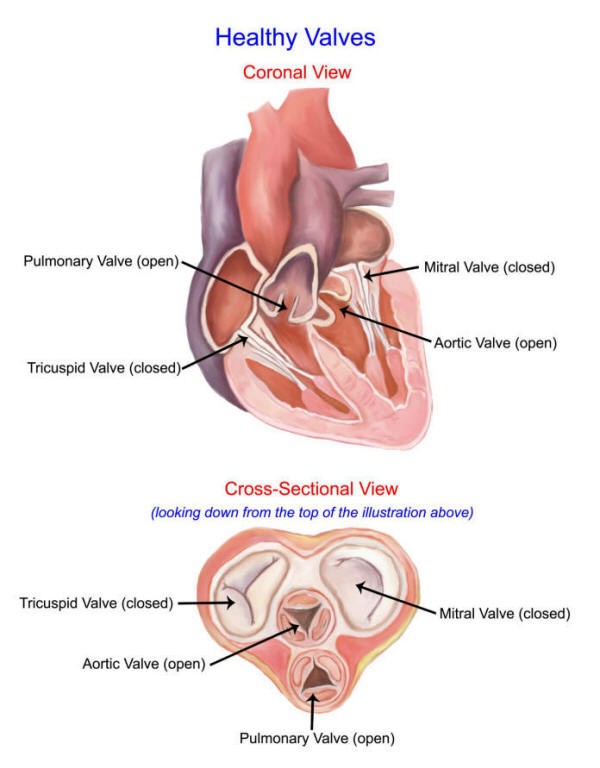
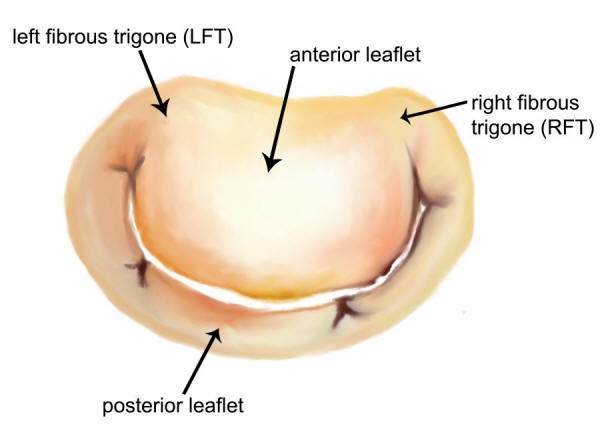
Now let’s take a closer look at the mitral valve.
In the picture below, notice there are two “leaflets” to the mitral valve:
- anterior leaflet
- posterior leaflet
Like any valve, the mitral valve can become either blocked (“stenosis”) or it can leak (“insufficiency”).
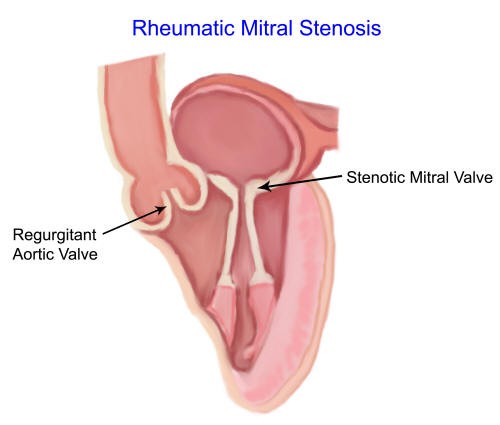
Mitral stenosis is fairly rare nowadays, since the advent of antibiotics. Previously, mitral stenosis was the most common valvular disorder in adults due to Rheumatic fever.
In Rheumatic heart disease, the mitral valve leaflets become thickened and begin to fuse to each other.
Below you can see a video testimonial from a young woman from Princeton, NJ, who had developed a rare type of severe mitral stenosis, along with tricuspid insufficiency, from underlying connective tissue disorders and an autoimmune disease process. She underwent mitral valve replacement and tricuspid valve repair.
Mitral Insufficiency
By far, the most common mitral valve problem today is mitral insufficiency – a leaking mitral valve. Here’s an animation of a leaking mitral valve:
There are several reasons why the mitral valve may be leaking:
Mitral Valve Prolapse
Although a commonly used term, it can apply to several different lesions. The pathology can range from simply having a slight excess or thinning of a particular leaflet, to having a disease process affecting both leaflets (Barlow’s syndrome) to having a torn leaflet or support structure (known as myxomatous degeneration of the valve). These are the most common indications for Mitral Valve Repair.
Mitral valve prolapse occurs when the mitral valve leaflets do not close tightly. There are a variety of causes of this problem. Over time, a leaky mitral valve can cause enlargement of the heart which can lead to heart rhythm problems, such as atrial fibrillation.
Mitral valve repair surgery remains the gold standard for correction of mitral valve prolapse.
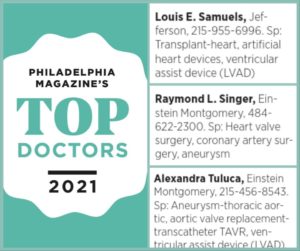
Recently, Jefferson Einstein Montgomery Hospital received a 3-Star Rating from the Society of Thoracic Surgeons for quality outcomes in patients who require isolated mitral valve surgery.
Below is the example of a 74-year-old patient who underwent mitral valve replacement surgery to treat her mitral valve prolapse. We also did radio-frequency ablation for her atrial fibrillation, and clip occlusion of her left atrial appendage to reduce her risk of stroke. Going home with a new valve, she left with normal rhythm, and no pain only 4 days after open-heart surgery!
Ischemic Cardiomyopathy
This is a fancy term that also applies to several different lesions. The most common is a patient with not enough blood supply to an area of heart muscle that provides the support structures to the mitral valve. In this instance, coronary artery bypass surgery may be all that is needed. By supplying fresh blood to the muscle, the function of the valve returns to normal. However, when the leaking is severe the valve can often be repaired.
A very serious complication from a heart attack can be the sudden loss of blood supply to the specialized muscle that holds the support structures to the mitral valve, the papillary muscles. In this instance, the papillary muscle ruptures and the patient has immediate congestive heart failure as a result of sudden, torrential leaking of blood across the mitral valve. Though there are reports of repairing papillary muscles, most surgeons will opt to replace the mitral valve in this very serious, life-saving emergency operation.
Lastly, a patient may slowly develop an enlarged heart from chronic heart failure. In this instance, as the heart enlarges the mitral valve becomes incompetent. The valve itself is completely normal, but the opening becomes gapping because of the ever enlarging heart. This is a controversial area. Some surgeons will opt for repair, while others will opt for replacement.
Ischemic Mitral Regurgitation (MR)
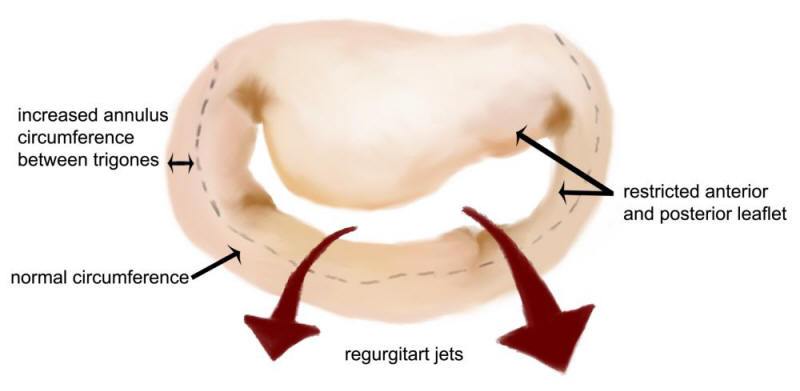
Ischemic mitral regurgitation (MR) is a frequent complication of myocardial infarction (MI), doubling the risk of developing heart failure and mortality. Its primary mechanism is leaflet tethering due to disturbed left ventricular geometry from myocardial scarring and remodeling of the heart as a result of the MI.
The incidence in the U. S. is impressive. Approximately 1 million people are diagnosed with a MI annually, with 50% developing ischemic mitral regurgitation. In patients with viable myocardium, coronary bypass surgery may reverse the left ventricular remodeling and improve the MR.
Unfortunately, 50% of patients with moderate or severe ischemic MR will have persistence or worsening of their mitral regurgitation after revascularization alone, requiring mitral valve surgery.
In this heart failure population, studies have shown that performing a mitral valve repair, using a restrictive annuloplasty ring, regrettably results in a 50% chance of recurrent, severe MR, at long-term follow-up —which leads to even poorer long-term survival. Therefore, a chordal-sparing valve replacement will likely provide a more durable result —and better outcomes— over mitral valve repair, in these critically I’ll patients.
Based on the current literature, and my personal experience, my choice of intervention for severe ischemic mitral regurgitation is to place a bovine mitral prosthetic valve, with concomitant clip occlusion of the left atrial appendage, due to the high risk of postoperative atrial fibrillation.
With the advent of valve-in-valve trans-catheter mitral valve replacement (TMVR), the patient will have a percutaneous option should the prosthetic valve leaflets deteriorate in the future. Indeed, sometime in the future, TMVR may become the standard of choice for the primary mitral valve operation.
Acute Mitral Regurgitation with Hemoptysis
The video below tells the story of a 32-year-old patient with an unusual combination of hypertrophic cardiomyopathy, along with aortic and mitral valve endocarditis, who presented late with acute mitral regurgitation and hemoptysis —coughing up blood.
Typically, acute mitral regurgitation presents with hemodynamic instability; however, it can present with extensive infiltrates of the lung, particularly on the right side, and alarming hemoptysis. This occurs as a result of acute pulmonary hypertension, resulting in alveolar hemorrhage that is accompanied by massive hemoptysis and acute respiratory failure.
From a surgical standpoint, this case was particularly challenging due to the patient’s underlying hypertrophic cardiomyopathy, along with the healed —but extensive—endocarditic damage to both the aortic valve and mitral valves. He underwent successful aortic valve repair and mitral valve replacement. He did not require a septal myectomy, as the left ventricular outflow tract (LVOT) gradient was only 4 mmHg at the end of the procedure.
The aortic valve was patched with native pericardium. The anterior mitral leaflet had been completely destroyed from the previous infection, and therefore a mechanical valve was selected for replacement due to the patient’s young age and history of hypertrophic cardiomyopathy.
He was discharged to home on post-operative day 6 on therapeutic warfarin therapy and 81mg aspirin daily.
Rheumatic Heart Disease
When a valve becomes blocked, it can also leak. The reason is simple: the valve is blocked but stays in a fixed position, never completely closing and never completely opening. As discussed above, almost all of these valves will need to be replaced.
Mitral Valve Repair
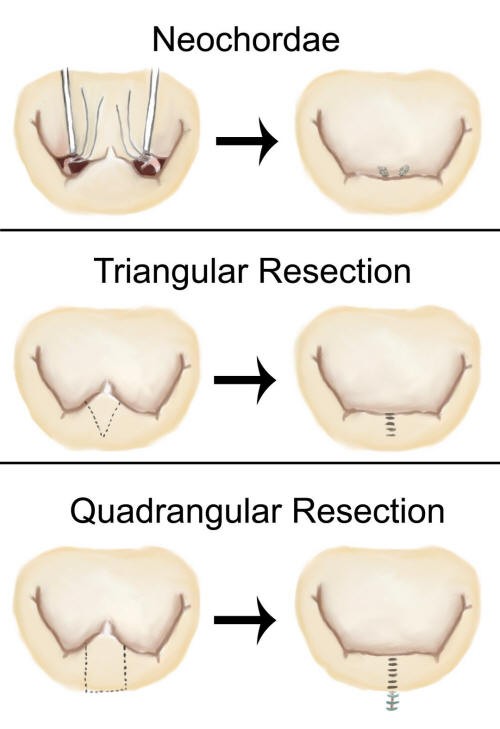
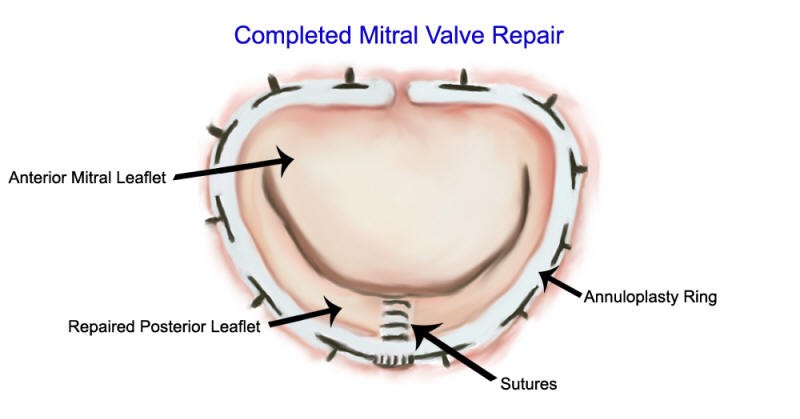
Below is a diagram of the different techniques of mitral valve repair.
After the valve is repaired, we place a ring around the repair known as an “annuloplasty ring.”
The history of mitral valve repair is quite interesting. Dr. Alain Carpentier began developing the techniques of mitral valve repair in Paris in the early 1970’s.
There were two reasons Professor Carpentier developed these techniques.
First, the early results of mitral valve replacement with prosthetic valves was poor. Unfortunately, surgeons didn’t fully understand the anatomy of the mitral valve at that time, especially the importance of the so-called sub-valvular apparatus (the papillary muscle and the attachments holding the mitral leaflets).
As a result, when surgeons placed prosthetic valves in the early days of heart surgery, they often used to cut out the leaflets and their attachments. This changed the geometry of the pumping chamber of the heart and resulted in a weakened heart muscle. Many of these patients died of heart failure after their valves were successfully replaced.
In addition, the use of blood thinners was not as standardized as it is today. Patients had many complications such as clotting of the prosthetic valves, stokes, and so on.
Second, Professor Carpentier began treating many poor patients from throughout Europe and Africa who suffered from Rheumatic heart disease and who would most certainly be non-compliant in taking their medications once they returned home. Therefore, regulating blood thinners in these patients was simply out of the question. By repairing their valves, these patients would not need blood thinners and would more likely survive with little medical follow-up.
Mitral valve repair, therefore is physiologically better than mitral valve replacement. As a result, we try to repair the mitral valve whenever possible.
Below you can view a video about the harrowing valve replacement experience of Mischel Satunas. It demonstrates some of the complications that can arise with Mitral Valve replacement. Fortunately there is a happy ending with the On-X Mitral Heart Valve:
Dr. Carpentier (next to me). Behind us is Dr. Charles Benoit, Chief at Geisinger Medical Center, Danville, PA
is mitral valve replacement bad?
No. As a follow-up to the development of mitral valve repair, an interesting parallel history occurred with mitral valve replacement with prosthetic valves: Surgeons better understood the anatomy of the mitral valve and began preserving the sub-valvular structures when
So, is it better to repair or replace the mitral valve?
Even though mitral valve replacement with a prosthetic valve is now completely safe, it is still always preferable to have the valve repaired if possible.
The reasons still remain the same. A repaired valve is physiologically closer to normal and the patient can avoid blood thinners. Though blood thinners are generally safe, they do have about a 2% yearly risk of complications. Plus, if you are on blood thinners, you have to have your blood level checked regularly.
But, mitral valve repair can be a complex procedure. Not every mitral valve can be repaired and not every repair works.
So, if you end up with a mitral valve replacement, it may be just what you need. You should not look upon this as a failure.
In my hands, approximately 90% of patients with mitral valve insufficiency will receive a repair. However, every patient and every valve is different. I prepare every patient for the possibility of needing a replacement valve even though I am going into the operation planning on repairing their valve.
I have had the privilege of taking multiple courses on mitral valve repair both in the United States and in Paris. I first visited Professor Carpentier in Paris in December of 1999 and became a Fellow in his Club Mitrale.
I received the ultimate honor of giving a presentation and sitting on a panel with Dr. Carpentier in Paris again in December 2011. Below is a picture of Dr. Carpentier and me during this presentation and panel discussion.
Professor Carpentier may be a little older but I can assure you that he is just as sharp as ever. This most recent trip to Paris was one that I will never forget. I am very grateful for all of his teaching. The other picture is the view from my hotel room! Paris is so beautiful. And, I love their bread and wine!
I have gotten to watch many of the true pioneers: In addition to Professor Alain Carpentier, I have had the privilege of meeting Dr. Carlos Duran, Dr. Delos Cosgrove, and Dr. Christophe Acar.
Here I am attending the 5th Biannual Mitral Conclave in New York City held May 2nd-3rd, 2019. It is the largest gathering of mitral valve surgeons from 61 countries around the world!

Mitral valve repair remains one of the most interesting and challenging open heart operations that we perform. Click here to view an interesting case – an example of Mitral Valve Repair!