What is Coronary Artery Bypass Surgery?
In patients with complex blockages of their coronary arteries that are not able to be treated further with medications or with angioplasty or the placement of a stent, your cardiologist may recommend coronary artery bypass surgery.
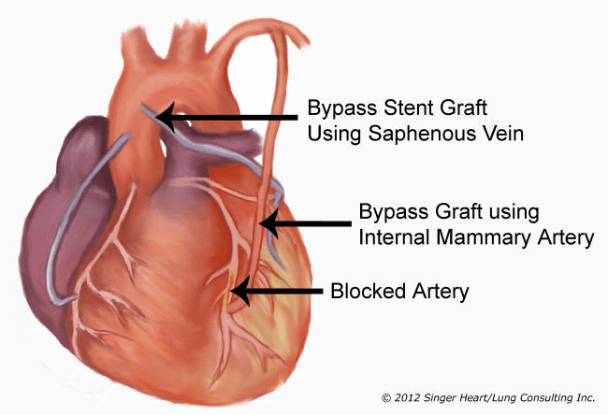
Coronary Bypass
A variety of surgical options:
Conventional Coronary Artery Bypass Surgery
Conventional coronary artery bypass surgery is still the best choice for the majority of patients. Though this is debated by some surgeons, the fact of the matter that conventional coronary artery bypass surgery has excellent results that are reproducible and unmatched so far by any of the newer, more radical approaches.
In the standard operation, an incision is made down the middle of the chest with an incision known as a median sternotomy. The incision does go through the midline of the sternum (breast bone) and at the end of the procedure, the sternum is put back together with stainless steel wires. The wires stay in the bone and you cannot feel them unless you are extremely thin.
Although this midline chest incision sounds pretty bad, the fact is that it is one of the most well-tolerated incisions that we make in patients. It turns out that there is no muscle in the midline of the chest and only a few cutaneous (skin) nerves.
Below you can hear the testimony of a patient who has undergone this procedure:
As far as the bone is concerned, once it is fixed at the end of the procedure, it causes very little discomfort. If you have ever had a broken bone (and I have had several) you would know that once a bone is “fixed” it no longer hurts. In fact, most patients complain very little about their chest incision, except for some feeling of numbness.
More importantly, the sternotomy incision gives the best exposure to all regions of the heart. This gives us the most choices if something unexpected occurs (which happens more often than not!). With a median sternotomy incision, your operation will not be compromised no matter what is found or needed to be done.
In conventional coronary artery bypass surgery, after the incision is made, the surgeon will make preparations to stop your heart by using the heart-lung machine. Below you can see a video of one of our perfusionists explaining the machine itself:
Why stop your heart?
The purpose is to provide a quiet, bloodless field in order to perform perfect sewing on your heart. And, in my mind, the single most important thing is to have perfect sewing. Perfect sewing will provide you with the best chance of a long-term good result.
What’s wrong with conventional coronary artery bypass surgery?
Nothing! Well, almost. Again, I strongly recommend conventional coronary artery bypass surgery to the majority of my patients who need coronary artery surgery.
In my hands, the success rate approaches 100% and the complication rate is less than 1%. However, like all procedures, there are indeed some risks.
In the case of conventional coronary artery bypass surgery, there are specific risks related to the use of the heart-lung machine. For example, in order to use the heart-lung machine, the surgeon must place tubes in the heart to drain the blood out to the machine and then other tubes to return the blood to the body after the heart-lung machine restores oxygen to the blood.
Although it’s rare, the sites were these tubes are placed around the heart can bleed, or even tear and cause life-threatening bleeding. Again, this is very rare.
Other risks of using the heart-lung machine include allergic reactions, kidney damage, and damage to the blood resulting in difficult clotting.
But perhaps the most concerning the risk of the heart-lung machine (and the most talked about in the media) is the risk of stroke and of mental status changes, such as memory loss and decrease in cognitive skills.
What’s the risk of stroke with the use of the heart-lung machine?
The answer depends on your age, the complexity of your procedure, and whether or not you have hardening of the arteries leading out of the heart and going to the brain, specifically the aorta in the chest and the carotid arteries in the head and neck.
As far as age alone is concerned, the risk of stroke is less than 1% in patients less than 70 years old, 1-4% in patients in their seventies, and 4-10% in patients over 80 years old.
To better assess your risk of stroke with conventional coronary artery bypass surgery, there are a number of screening tests that we perform on all of our patients.
First, and foremost, we perform a physical examination listening for murmurs (also known as bruits) over the neck arteries (carotid arteries). Then we perform what is known as a carotid ultrasound which can visualize if there are blockages in the arteries going to your head.
Lastly, in the operating room, we can feel your aorta to determine if it is hard from plaque and we can perform an ultrasound directly on the aorta to look for plaque.
If we find that the aorta or the carotid arteries are diseased, we can alter the operation so as to minimize your risk of stroke during your heart operation.
This extensive screening procedure has greatly reduced our incidence of stroke with conventional coronary artery bypass surgery.
How about memory loss or decrease in cognitive skills?
The jury is still out on this issue.
There was a significant article published in the New England Journal of Medicine that got a lot of attention in the media. That article suggested the patients who underwent conventional coronary artery bypass surgery with the use of the heart-lung machine exhibited signs of early dementia. Personally, I did not feel the article was conclusive.
Most of the patients were elderly to begin with and it would be impossible to determine whether or not they would have developed dementia if they did not have heart surgery.
Clearly, patients complain of some emotional and perhaps even intellectual changes during the first 6 months after surgery.
In fact, we can measure a protein (protein S100) that is decreased after the use of the heart-lung machine but returns to normal levels soon after recovery.
Protein S100 may be involved with memory and other cognitive skills.
However, testing at 6 months has shown that protein S100 levels return to normal in most patients as does all of their cognitive testing.

My mother holding her granddaughter shortly after conventional heart surgery!
I can tell you this much: my mother underwent a valve replacement and 2 bypasses at age 78. On the way home from the hospital she insisted that I drive her to my father’s tavern so that she could catch up with the bookkeeping.
At age 80, she continued to run my father’s tavern, plus she sold real estate part-time and played tournament bridge. On top of that, she would drive herself down to the casinos in Atlantic City on Sundays to deliver my inheritance to Donald Trump! And, once a month or so, she traveled to New York to see Broadway shows and have lunch and dinner!
Median Sternotomy
Now, let’s talk about the conventional incision, the median sternotomy.
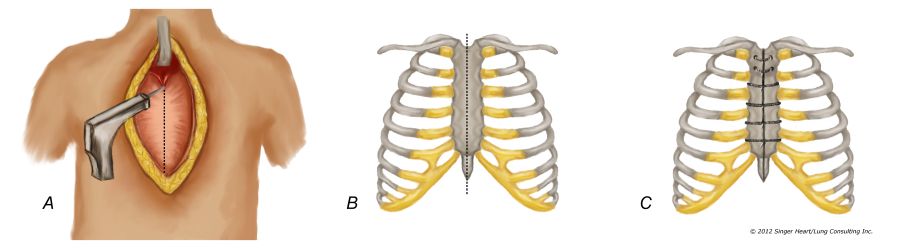
The dotted lines below show where the median sternotomy incision is made.
Next, the sternal bone (breast bone) is divided with a power saw.
At the end of the procedure, the sternum is put back together with stainless steel wires.
Median Sternotomy
Median Sternotomy: Friend or Foe?
Much of the debate on minimally invasive heart surgery surrounds the size and location of the incision.
Although the median sternotomy (anterior chest incision with splitting) sounds bad, it is actually surprisingly well-tolerated and, most of all, is an excellent incision.
Why is it an excellent incision?
- It provides excellent exposure to all regions of the heart.
- It allows for the unexpected events that can occur during any surgery and allows the surgeon to address any unexpected event immediately and safely.
- It is an incision that is easy to perform.
- Most of all, as I stated above, it is surprisingly well-tolerated by the patient.
Reasons the anterior midline chest incision is so well tolerated:
- There are no muscles to cut through in the midline of the chest.
- There are no large nerves.
- As far as the bone is concerned, once a broken bone is “fixed” it not longer hurts.
- Overwhelming, most patients have remarkably little discomfort and no limitations as a result of the conventional sternotomy incision.
The median sternotomy incision, like all incisions, is not without risks. Some of these risks include wound infections, though infections can occur in any wound.
Advocates of smaller, lateral incisions say that these incisions allow patients to return sooner to work or to an active lifestyle.
This has never been shown in any of the studies of MIDCAB, OPCAB, Heartport, or now Robotics.
Indeed, not only does the lateral chest incision gives limited exposure due to the limitation of the ribs but it is can be associated with tremendous pain because of injury to the intercostals nerves that run beneath each rib.
One story provides a good example:
I operated on a young patient who had a very small 4-inch incision under her breast to repair a simple atrial septal defect using Heartport® techniques.
She complained for 6 months of intercostal nerve pain. That same day I operated on a 80-year-old patient who had a much more complex procedure through a conventional median sternotomy incision who had absolutely no pain and was seen in the office one time after the surgery and never needed to return to the office again.
More Testimonials:
Below you can listen to more testimonials from patients.
In the first one, you can hear from Mike after his triple bypass surgery (CABG). Only day three and he has no pain after the conventional method.
In the second one, Earl demonstrates how, with newer techniques for cardiac anesthesia and surgery, post-operative pain can be minimized, allowing patients to ambulate sooner, and most importantly, get home sooner.
In the third you can hear from Dennis, a patient of mine who had quadruple bypass via median sternotomy. He is only four or five hours post-op in this video!
Bottom line on conventional coronary artery bypass surgery…
If I needed coronary artery bypass surgery… and if my surgeon determined that I did not have excessive risk factors for stroke… I would absolutely demand that I undergo conventional coronary artery bypass surgery!
On the Society of Thoracic Surgeons website, you can read more about how open heart surgery outperforms stents in patients with multivessel disease.
Click here to learn about less invasive coronary bypass….
“All things must change to something new, to something strange.” – Henry Wadsworth Longfellow