Atrial fibrillation is the most common cardiac arrhythmia. Indeed, over 2 million people in the United States have atrial fibrillation. While once thought to be harmless, it is now known that atrial fibrillation can increase the risk of stroke up to sevenfold.
There are a variety of approaches to treat atrial fibrillation, from medications to catheter-based ablation, as well as newer minimally invasive surgical procedures.
Atrial fibrillation is a complicated arrhythmia for which the cause is not completely understood. The most common theory is that multiple circuit reentry causes the electric charges in the atrial chambers to go in all different directions. Thus, the atrial chambers “fibrillate” instead of contracting in a uniform fashion.
Atrial fibrillation adversely affects the overall function of the heart and is associated with increase complications and increase risk of death. For example, blood clots can form in the atrium because the atrial fibrillation just swirls the blood around in the chamber instead of ejecting it in a uniform manner. These blood clots can break loose and travel to the brain causing a stroke. Most patients with atrial fibrillation therefore require lifelong anticoagulation with blood thinners such as Coumadin ®.
The Maze Procedure
The Maze procedure was designed to interrupt the multiple reentrant circuits that causes the atrial chambers to fibrillate.
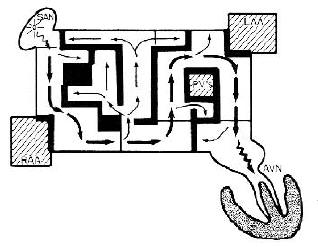
Conceptual Design of the Maze Procedure
Convergent or “Minimally Invasive” Maze Procedure
There have been a lot of exciting advances within the Maze Procedure. One such advancement is called the “Convergent Maze Procedure.” This method is minimally invasive. It combines electrophysiology (EP) and cardiac surgery treatments to restore the normal heart rhythm.
I’m the only surgeon in Philadelphia performing a high volume of this procedure. It is suitable for patients who have suffered a long time from arrhythmia sufferers but have have little success with other treatments. This procedure is also appropriate for those with structural heart disease.
The procedure entails my reaching the heart by inserting a video-assisted scope into your upper abdomen via a small 1-inch incision. Then, by using radiofrequency ablation (which is just focused heat) I will create scar tissue in the problem area. This scar tissue will then blocks the abnormal electrical signals, thus restoring the natural rhythm of your heart.
Most of my patients who have had this procedure no longer need to take heart rate and rhythm medications afterwards. Hospital stays seldom go beyond three days.
Cox-Maze Procedure
Dr. James L. Cox, the now-retired Professor and Chairman, Department of Thoracic and Cardiovascular Surgery at Georgetown University Medical center is the father of surgery for atrial fibrillation. Dr. Cox began developing operations to treat atrial fibrillation in the early 1980’s.
The basic concept of the Cox-Maze procedure for atrial fibrillation was to create multiple incisions in the left and right atrium and then sew them back up immediately causing a full-thickness scar in the pattern of a maze. The maze would interrupt the reentry circuit and force all of the electricity to go in one direction, just as if you were walking through a maze.
Studies continue to show that mitral valve surgery can be safely performed in most elderly patients with severe mitral regurgitation. Mitral valve repair techniques, combined with the Cox Maze IV procedure to correct atrial fibrillation, and placement of an occlusive clip on the left atrial appendage, can markedly improve patients’ quality of life.
Moreover, many patients can have their chronic anticoagulation stopped, decreasing the risk of complications associated blood thinners.
The best outcomes occur when operative intervention is performed early, before advanced symptoms of heart failure develop.
Below you can hear the testimony of a patient who had an AtriCure left atrial clip to occlude the left atrial appendage. This decreases the risk of stroke for patients with atrial fibrillation.
Radio-Frequency Maze Procedure
An advance in the Maze Procedure has been the use of a variety of energy sources to create scars in the atria without the need to make incisions. Radio-frequency energy is the most popular, but other energy sources include microwave, laser, and even freezing the tissue (cryo-ablation).
Eliminating all of the cutting and sewing in the atria greatly shortens and simplifies the operation and greatly reduces the risk. Now, a complete Maze procedure using the radio-frequency technique can take as little as 20 minutes (not including the time to open and close the chest).
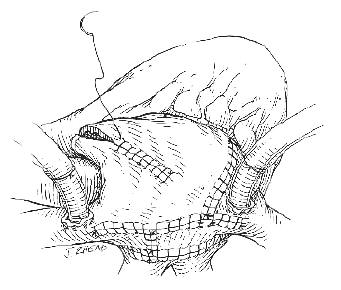
Incisions and Suturing for the ORIGINAL Cox-Maze Procedure
The most common indication for radio-frequency Maze procedure is during mitral valve repair, since many patients with mitral valve disease have developed atrial fibrillation.
Below is the equipment I use when I perform radio-frequency Maze procedure. The machine generates the radio-frequency energy which is transmitted to a variety of instruments that are placed both inside and outside of the atria to create the Maze lesions.
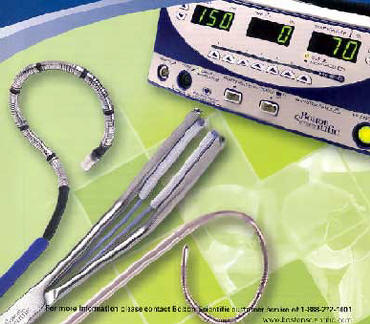
Equipment for the Radio-Frequency Maze Procedure
Our experience with the Maze procedure is growing. Minimally invasive approaches are being investigated as well as new instruments and energy sources. This is certainly one of the most interesting and most exciting areas of cardiac surgery.
Below you can hear the testimony of a lovely 86-year-old patient from Allentown, Pennsylvania who underwent successful double-valve open-heart surgery, combined with radio-frequency maze procedure for atrial fibrillation.
She also had clip occlusion of her left atrial appendage. Prior to surgery, she couldn’t walk 6 steps without needing to stop due to shortness of breath.
After only 5 days post-op, she was ready to be discharged. in addition to having her heart failure corrected, she no longer requires anticoagulants which is beneficial to reducing bleeding complications in elderly patients.
Below is a video interview is with a 75-year-old patient, on postoperative day #3, after a surgical aortic valve replacement surgery for critical aortic stenosis, combined with a radiofrequency maze procedure for atrial fibrillation.
His aortic valve was replaced with a 25mm Edwards Inspiris Resilia bovine bioprothetic valve. The maze procedure was performed with the AtriCure radiofrequency system, along with placement of a 50mm AtriCure left atrial clip occluder.
The maze procedure treats atrial fibrillation by creating a specific pattern (maze) of scar tissue, redirecting the reentrant electrical currents that cause atrial fibrillation. Clip occlusion of the left atrial appendage reduces the risk of embolic stroke from afib. The success rate for a maze procedure is 80 to 90%, and is well-tolerated.
The patient is being discharged on postoperative day #3, with minimal to no discomfort and in normal sinus rhythm. Surgical aortic valve replacement, combined with a maze procedure, can be performed through a conventional median sterneromy with minimal pain, short lengths of stays, and early recovery.
𝘕𝘰𝘵𝘦: 𝘛𝘩𝘦 𝘱𝘰𝘴𝘵𝘪𝘯𝘨 𝘰𝘧 𝘵𝘩𝘪𝘴 𝘷𝘪𝘥𝘦𝘰 𝘸𝘢𝘴 𝘱𝘦𝘳𝘧𝘰𝘳𝘮𝘦𝘥 𝘸𝘪𝘵𝘩 𝘸𝘳𝘪𝘵𝘵𝘦𝘯 𝘱𝘦𝘳𝘮𝘪𝘴𝘴𝘪𝘰𝘯 𝘧𝘳𝘰𝘮 𝘵𝘩𝘦 𝘱𝘢𝘵𝘪𝘦𝘯𝘵. 𝘐 𝘩𝘢𝘷𝘦 𝘯𝘰 𝘧𝘪𝘯𝘢𝘯𝘤𝘪𝘢𝘭 𝘳𝘦𝘭𝘢𝘵𝘪𝘰𝘯𝘴𝘩𝘪𝘱 𝘸𝘪𝘵𝘩 𝘦𝘪𝘵𝘩𝘦𝘳 𝘌𝘥𝘸𝘢𝘳𝘥𝘴 𝘓𝘪𝘧𝘦 𝘚𝘤𝘪𝘦𝘯𝘤𝘦𝘴 𝘰𝘳 𝘈𝘵𝘳𝘪𝘊𝘶𝘳𝘦.
AtriClip PRO2 Device by AtriCure Corporation
Illustrated here is my approach using a thoracoscope and a 2-inch of incision to apply a permanent clip to completely to occlude the left atrial appendage —(AtriClip PRO2 Device by AtriCure Corporation).
Along with a minimally invasive subxiphoid radiofrequency surgical ablation technique, patients like this 68-year-old can be restored back to normal sinus rhythm and taken off anticoagulant medications! By occluding the left atrial appendage, the risk of stroke for patients in a fib is markedly reduced!
Case Studies
Complex Repair In Older Patients
Mitral valve repair surgery can be successfully performed in older patients who require concomitant coronary artery bypass surgery.
As in many patients with severe mitral valve prolapse and regurgitation, this 77-.year old patient had also developed atrial fibrillation. Therefore, we combined the mitral valve repair operation with both a coronary bypass surgery and a radio-frequency maze procedure, to correct his rhythm back to normal.
With permission from the patient to post, the patient is hemodynamically stable postop, with a well-repaired mitral valve, normal biventricular function, and his normal sinus rhythm has been restored.
In addition, as part of the maze procedure, an AtriCure clip was placed at the base of the left atrial appendage. This will allow the patient to enjoy a low risk of stroke in the future, even if the a-fib returns. In addition, the patient will no longer require blood thinners for atrial fibrillation in the future.
For patients, it’s important to know that higher volume surgeons are more likely to repair a mitral valve than to replace it, regardless of the patient’s age, or need for other procedures. This is why it’s important for patients to seek second opinions and to ask questions about their surgeon’s experience and outcomes.
concomitant bi-atrial Cox-Maze IV procedure
This is a case of mitral valve repair and tricuspid valve repair with a concomitant bi-atrial Cox-Maze IV procedure, performed through a conventional sternotomy approach. (Shared with the patient’s permission to post).
🔹 Why repair the tricuspid valve? Whenever the tricuspid annulus is greater than 40 mm, concomitant repair is essential. Leaving it unaddressed risks progressive annular dilation, worsening tricuspid regurgitation, and ultimately poorer outcomes—even if the primary focus is the mitral valve. Early and decisive tricuspid intervention helps secure long-term valve competence.
🔹 Why a complete bi-atrial Maze procedure? A comprehensive Cox-Maze IV—not a partial or limited ablation—is crucial in restoring and maintaining durable sinus rhythm. By fully addressing both atria, we maximize the chances of long-term freedom from atrial fibrillation and reduce the risk of stroke, heart failure, and late arrhythmia recurrence.
🔹 The bigger picture: While such procedures are undoubtedly complex, combining valve repair with a full Maze procedure delivers the best short- and long-term outcomes for patients.
Meticulous, all-encompassing surgical strategies translate into durable valve function, improved rhythm control, and better quality of life.This case highlights how completeness matters in cardiac surgery—not only for immediate success but for sustained results years down the road.