Barlow’s Disease is a specific form of degenerative mitral valve disease characterized by myxomatous degeneration of the mitral valve, leading to mitral valve prolapse (MVP) and severe mitral regurgitation.
Barlow’s Syndrome is a relatively common condition that may result in the leaftlets of the mitral valve bulging into the left atrium of the heart, just as the valve closes during ventricular contraction. This abnormality is due to degeneration of the tissue, causing the mitral valve leaflets to become stretched and enlarged. The redundant tissue prevents the valve from closing properly, often resulting in prolapse of the mitral leaflets and mitral valve regurgitation.
Barlow’s syndrome occurs in 1% to 6% of otherwise normal populations. However, people with Graves’ disease, Marfan’s syndrome, Duchenne muscular dystrophy, myotonic dystrophy, sickle cell disease, and rheumatic heart disease have a higher incidence of this condition.
Symptoms can include fatigue, migraines, dizziness, panic attacks, low blood pressure, shortness of breath, palpitations, and chest pains that are not associated with angina.
The diagnosis and degree of mitral regurgitation is determined by echocardiogram. More specific morphology of the mitral valve can be analyzed by transesophageal echocardiogram (TEE), especially when planning for mitral valve repair surgery.
Mitral valve repair surgery can be done successfully in more than 95% of cases, without the need to replace the valve.
1. Pathology
- Thickened, redundant, and elongated mitral valve leaflets
- Excessive leaflet tissue with billowing or prolapsing segments
- Common involvement of both anterior and posterior leaflets
-
Chordae tendineae may be elongated, thickened, or ruptured
2. Clinical Presentation
- Can be asymptomatic for years
- Symptoms (when present): Dyspnea (shortness of breath), Fatigue, Palpitations, Atypical chest pain
- Severe cases may exhibit heart failure symptoms
3. Diagnosis
- Best identified with echocardiography, especially 3D TEE
- Echo findings include prolapse of thick, bulky leaflets, mitral annular dilatation, and systolic “bowing” of leaflets into the left atrium
- Severe, often eccentric, mitral regurgitation may be observed
-
Additional findings may include annular disjunction or posterior leaflet flail
4. Surgical Considerations
- Complex anatomy makes repair more challenging than in fibroelastic deficiency (FED)
- Repair by an experienced mitral valve surgeon is preferred over replacement
-
Techniques may involve resection or remodeling of excess leaflet tissue, chordal transfer or artificial chordae (Gore-Tex), and the use of an annuloplasty ring to restore shape and function
5. Prognosis
- Excellent long-term outcomes with repair by experienced surgical teams
- Without repair, progressive regurgitation can lead to left ventricular dysfunction, atrial fibrillation, and heart failure.
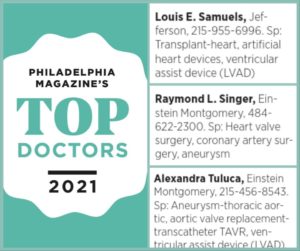
If you’ve been diagnosed with Barlow’s Mitral Valve Disease, it’s important to see a surgeon who has experience repairing this complex, degenerative form of mitral valve prolapse, typically prolapse that involves both mitral leaflets.
The complexity of surgical lesions in patients who have bi-leaflet prolapse often include excessively thick and billowing leaflet segments, chordae tendineae elongation and/or rupture, and severe dilation of the valve as well as the heart chambers. Many patients will develop atrial fibrillation, as their heart chambers enlarge.
Case Studies/Testimonials
This video was taken in the operating room during a complex mitral valve repair operation for bi-leaflet valve prolapse in a patient with Barlow’s Mitral Valve Disease.
In this video, I show the anatomy of the underlying pathology as well as explaining how we were able obtain a successful repair.
Remember, it’s important to ask your surgeon how many mitral valve repair operations they perform yearly and also their success rate. A qualified surgeon should perform more than 25 mitral valve repairs per year with a repair rate of greater than 95% rather than replacing the valve with an artificial one. Always better to have your mitral valve repaired!
Most important of all, never hesitate to ask for a second opinion!
This video illustrates a case of a 60-year-old man with Barlow’s syndrome, who underwent a successful mitral valve repair operation, utilizing pledged 5–0 Gore-Tex neo-chord sutures through the prolapsed posterior mitral valve leaflet, along with placement of a 36mm Edwards Physio-I mitral angioplasty ring.
A 50mm AtriCure AtriClip was placed at the base of the left atrial appendage to occlude it and thus reduce the risk of potential stroke from post-operative or future bouts atrial fibrillation.
Barlow’s Disease is a type of degenerative mitral valve disease where the valve leaflets become thickened, redundant (excess tissue), and often floppy. This leads to prolapse of the valve leaflets into the left atrium during systole (heart contraction), which can cause mitral regurgitation (leaking of blood backward into the atrium). Go
This video is of a 71-year-old with Barlow syndrome, excessive leaflet tissue, bi-leaflet prolapse, and there’s a torn cord of the posterior leaflet. The TEE shows the severe mitral regurgitation and the bi-leaflet prolapse. You can see the preoperative three-dimensional study showing severe mitral regurgitation and the bi-leaflet prolapse.
The 2D view is of the mitral valve repair. You can see there’s no further mitral regurgitation. The valve opens well, and there’s no systolic anterior motion. Biventricular function is excellent. The 3D of the final repair shows there’s zero residual mitral regurgitation and despite being dilated from the chronic mitral regurgitation, all the segments are moving well, and she has overall normal biventricular function.
With permission from this patient to post, this 47-year-old man developed sudden severe mitral regurgitation and atrial fibrillation due to Barlow’s Syndrome—excess mitral leaflet tissue, bi-leaflet prolapse, with rapid atrial fibrillation. His symptoms included extreme lethargy and shortness of breath.
He underwent a complex bi-leaflet mitral valve repair and a radio-frequency maze procedure via a median sternotomy, including a clip occlusion of the left atrial appendage to prevent the risk of embolic strokes in the future.
UPDATE (Second Video):
Six months later Nick discusses his recovery after mitral valve repair surgery and Cox-Maze IV procedure for severe mitral valve prolapse. This 47-year-old patient shares insights into his journey post mitral valve repair surgery and Cox-Maze IV procedure for severe mitral valve prolapse and atrial fibrillation.
A recent 6-month echocardiogram indicates no residual mitral regurgitation, a minimal gradient across the repair, and the maintenance of a regular sinus rhythm. Additionally, the patient’s incision has healed well, giving him a pain-free experience during daily activities and exercise.
Surgeons must continue to monitor their valve repair patients to ensure long-term quality outcomes.
60-year-old patient with a heart murmur for many years was diagnosed with mitral valve prolapse six years ago. She was on medication for the heart murmur and was diagnosed with an echocardiogram, at which time they discovered the mitral valve prolapse in both leaflets. The cardiologist suggested surgery, but the patient wanted a second opinion due to her hesitance. It was recommended that she have an echo every six months.
Then, the patient began to feel unwell with shortness of breath. Her doctor moved the surgery window from six months to four months to check on it. The patient decided to have the surgery. It was noted that her heart was already getting a little bit enlarged, which caused concern, as that is one of the
indications of severity. She was diagnosed with Barlow’s syndrome, or Barlow’s disease, which is excessive tissue of both leaflets, know as bi-leaflet prolapse. We had to repair the anterior leaflet and the posterior leaflet, and put a ring in, and we did a follow-up echo, not only in the operating room, but also right before discharge yesterday. The echo was perfect. She has no further mitral leakage nor stenosis. She does have SAM, systolic anterior motion, because she has an asymmetric septal hypertrophy (a little extra muscle knuckle).
She was discharged four days after surgery and says the pain after her conventional sternotomy is minimal.